Optimizing Drug Design: The Synergy of Tissue Distribution & PK
Ram Shankar Upadhayaya
Visionary Pharma Leader | Oncology Drug Discovery Expert | Molecular Oncologist | Clinical Trial Strategist | Translating Science into Medicines | Strategic Alliances and Global Business Development
Given the budgetary constraints in drug discovery and development, mapping scientific studies with uncompromised data quality requires smart decision-making to maximize return on investment (ROI). For biotech companies, every study must serve both scientific and business objectives-establishing proof of concept (PoC), supporting regulatory submissions, and instilling confidence in investors. Tissue distribution studies play a crucial role in determining a drug’s efficacy, safety, and pharmacokinetic profile, but when and how to conduct them remains a key strategic decision.
By integrating tissue distribution with early-stage pharmacokinetics (PK) studies, companies can minimize costs and reduce animal usage while ensuring high-quality data. With regulatory agencies like the FDA focusing on modernization and animal-use reduction, it is essential to explore cost-effective yet scientifically robust approaches, such as serial sampling and optimized study designs, to make informed decisions that align with both financial constraints and regulatory expectations.
A. Tissue Distribution
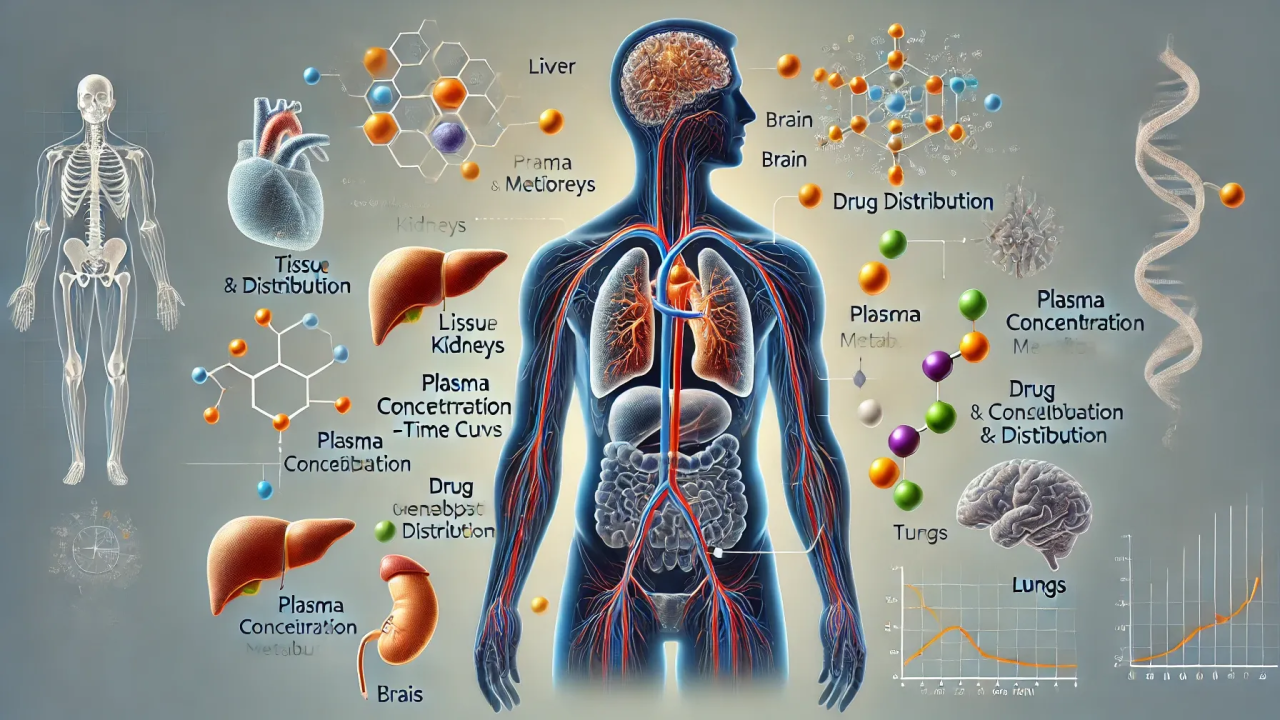
Tissue distribution refers to the process by which a drug or its metabolites distribute across different organs and tissues after administration. For small molecules, factors such as lipophilicity, plasma protein binding, and passive diffusion influence their distribution, while biologics rely more on receptor-mediated uptake, FcRn recycling, and tissue-specific permeability barriers. This critical parameter helps determine a drug's efficacy, potential toxicity, and pharmacokinetic (PK) profile, ultimately influencing dosage regimens and therapeutic windows. The distribution varies significantly between small molecules and biologics, with factors such as molecular weight, lipophilicity, and protein binding playing crucial roles.
Why is Tissue Distribution Important?
When Should Tissue Distribution Be Considered?
B. Optimizing Tissue Distribution Studies for Cost-Effectiveness?
1. Integrating with Initial PK Studies
Performing tissue distribution studies alongside PK studies (e.g., 2 mpk IV and 10 mpk PO doses, which are commonly used in early-stage studies for small molecules but may differ for biologics) can improve efficiency. However, initial PK studies often do not provide adequate drug concentrations in tissues to establish dose proportionality. This raises the question: should companies invest in additional studies later or optimize early-stage planning?
2. Serial Sampling vs. Non-Serial Sampling
One way to reduce animal use and cost is to adopt serial sampling methods in cannulated mice, particularly in studies where frequent blood sampling is needed to track pharmacokinetics over time. This approach is more feasible in small molecule studies due to their rapid clearance rates, whereas for biologics, factors such as target-mediated drug disposition and extended half-lives may present challenges. Additionally, while serial sampling reduces inter-animal variability, it requires specialized surgical expertise and infrastructure, making it a trade-off between precision and logistical feasibility. The choice between serial and non-serial sampling has key trade-offs:
Pros of Serial Sampling:
Cons of Serial Sampling:
3. Saving Organs for Future Biodistribution Studies
A common discussion in biotech companies is whether to preserve organs from PK studies for later biodistribution analysis. This approach could save resources and avoid additional animal studies, but potential drawbacks exist:
Pros:
Cons:
C. Serial Sampling vs. Traditional Approaches
One of the pressing questions is why many pharma companies still rely on traditional non-serial sampling despite the cost-effectiveness of serial approaches. The possible reasons include:
D. Aryastha's Recommendations
Conclusion
Small biotech companies face difficult decisions in balancing cost, regulatory compliance, and scientific quality. A notable example is a biotech startup that successfully optimized its tissue distribution strategy by integrating PK studies with biodistribution assessments, minimizing animal use and reducing costs while maintaining high-quality data.
This approach not only streamlined their regulatory submission but also demonstrated that early-stage strategic planning can significantly enhance efficiency in drug development. A well-thought-out approach to tissue distribution, integrating PK studies and considering serial sampling, can optimize resource use without compromising the quality of the data. As regulatory agencies move toward minimizing animal testing, innovative study designs will play a crucial role in shaping the future of drug development.